BLEEDING
Bleeding
A frequent question we receive in our support group is, “ I had my ovaries removed, but I still have my uterus. Why am I bleeding?”
This is a common problem for women who are in Surgical Menopause who have opted to keep their uterus and are either on a continuous combined HRT regiment (continuously taking both estrogen and progesterone in an attempt to suppress the growth of the uterine lining) or those women who are on hormone cycling (taking cycles of progesterone intermittently to induce the shedding of the uterine lining while on a continual dose of estrogen).
Bleeding and Continuous Combined HRT
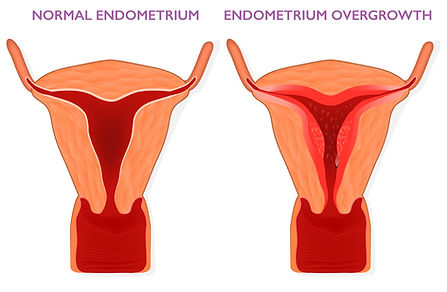
In the case of women who are in Surgical Menopause, have kept their uterus and opted for a continuous HRT regiment, the issue of bleeding becomes a problem if the amount of progesterone they are taking is not sufficient to oppose the amount of estrogen they are taking and thus their uterine lining has grown too thick causing unscheduled spotting or bleeding.
The bleeding these women experience is an indicator that the uterus is no longer being adequately protected by progesterone, which is its primary job in women with a uterus on continuous combined HRT. Over time this situation, if not properly addressed, can put a woman at risk for uterine cancer. According to studies, in a postmenopausal woman with vaginal bleeding, the risk of cancer is approximately 7.3% if her endometrium is thicker than 5 mm. Because of the risk of uterine cancer, it is important that you discuss treatment and solutions with your doctors when you first notice the bleeding. Typically the first step will be to have a transvaginal ultrasound so your doctor can measure the thickness of your uterine lining and determine what the next best step would be for treatment.
There are four primary solutions that currently exist for women who are experiencing this type of bleeding from uterine lining overgrowth. They can consult with their doctor and:
-
Up their progesterone dose to reduce the thickness of the uterine lining and prevent further breakthrough bleeding. The downside to this option is that in order to accomplish this women must take unusually high doses of progesterone, deliberately inducing hormone imbalance in the body, and often bringing on some of the unwanted side effects from taking too much progesterone such as depression, weight gain, water retention and mood disorders.
-
Change the delivery method of their progesterone to either vaginal progesterone or a hormonal IUD (Intrauterine Device) such as Mirena or Skyla. Which has proven the most effective in keeping uterine lining thin and healthy as it is inserted directly into the uterus and the hormones are localized to the uterus. It also boasts the advantage of not affecting systemic estrogen.
-
Consider taking Duavee which is an oral HRT that contains both conjugated synthetic estrogens and bazedoxifene. The advantage of taking bazedoxifene is that it blocks estrogen from reaching cells in the uterine lining, and thus it is able to protect against overgrowth of uterine tissue.
-
A final line of defense for women whose uterine lining has grown too thick is to undergo a D and C or a Dilation and Curettage. This is a procedure that is done in the hospital under anesthesia in which the cervix is dilated and the uterine lining is scraped and scooped out with a curette.
Bleeding with Hormone Cycling
Women with a uterus in Surgical Menopause who experience spotting or bleeding while on a hormonal cycling regiment of HRT typically experience this problem when they are spacing out their cycles of progesterone too far or the dose of progesterone they are taking during their hormone cycles is not strong enough to shed all of their uterine lining.
When this is the case the first action you should take would be to discuss the spotting or bleeding with your treating physician. Most often your doctor will request a transvaginal ultrasound to measure the thickness of your uterine lining to determine what treatment or alterations to your hormone cycling regiment need to take place.
If the transvaginal ultrasound reveals that your uterine lining is thicker than it should be, then you and your doctor will likely discuss shortening the duration between cyclical bleeds or increasing your dose of your progesterone during your cyclical bleeds so as not to allow the uterine lining to grow too thick, for a thick uterine lining puts you at risk for uterine cancer. You may also consider the above mentioned method of continuous combined hormone cycling as an alternative to cyclical bleeds induced by progesterone.



